Amniocentesis
 Amniocentesis is a procedure
used to obtain a small sample of the amniotic fluid that surrounds the fetus to
diagnose chromosomal disorders and open neural tube defects (ONTDs), such as
spina bifida. An amniocentesis is generally offered to women between the 15th
and 20th weeks of pregnancy who are at increased risk for chromosome
abnormalities, such as women who are over age 35 years of age at delivery, or
those who have had an abnormal maternal serum screening test, indicating an
increased risk for a chromosomal abnormality or neural tube defect.
Amniocentesis is a procedure
used to obtain a small sample of the amniotic fluid that surrounds the fetus to
diagnose chromosomal disorders and open neural tube defects (ONTDs), such as
spina bifida. An amniocentesis is generally offered to women between the 15th
and 20th weeks of pregnancy who are at increased risk for chromosome
abnormalities, such as women who are over age 35 years of age at delivery, or
those who have had an abnormal maternal serum screening test, indicating an
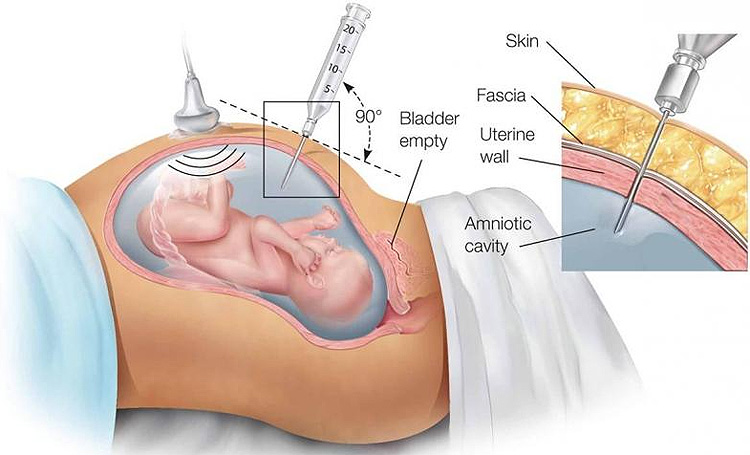
increased risk for a chromosomal abnormality or neural tube defect.- The woman's abdomen is cleansed with an antiseptic
- The doctor may or may not give a local anesthetic to numb the skin
- Ultrasound is used to help guide a hollow needle into the amniotic sac
- A small sample of fluid is withdrawn for laboratory analysis
- Strenuous activities should be avoided for 24 hours following an amniocentesis
- Women may feel some cramping during or after the amniocentesis
Women with twins or other multiples need sampling from each
amniotic sac, in order to study each baby. Depending on the position of the
baby, placenta, amount of fluid, or patient's anatomy, sometimes the
amniocentesis cannot be performed. The fluid is sent to a genetics laboratory
so that the cells can grow and be analyzed. Alpha-fetoprotein, a protein made
by the fetus that is present in the fluid, is also measured to rule out an open
neural tube defect, such as spina bifida. Results are usually available in
about 10 days to two weeks, depending on the laboratory.
Many women are understandably concerned about the potential
risk for miscarriage associated with amniocentesis. And, while it’s true that
increased miscarriage risk was once a significant concern, advancements in the
technology for performing this procedure have significantly reduced this
risk.Currently, the risk of miscarriage for amniocentesis is about 1 in 400
pregnancies, with the risk occurring due to infection or premature labor
induction. However, as with of all causes of miscarriage, it’s really
challenging to connect miscarriage with one specific event, like getting an
amnio done. Also, with the use of guided ultrasound imaging, there is little
risk of injury to the developing baby.Signs of complications that warrant
immediate medical attention are watery or foul odour in pregnancy discharge,
contractions, severe pain, and signs of infection like fever and flu-like
symptoms. Some light spotting after an amnio can be expected, but continuous
severe bleeding is also a sign to immediately see a medical professional.
An amniocentesis can be really informative because it can
help you plan for what to do if the fetus requires additional surgery (like
fetal surgery for spina bifida) and help you address additional resources you
might need for the baby. However, some women choose not to get the procedure because
they will carry the baby to term regardless of the results of the
amniocentesis. Depending on your own personal preferences and moral
philosophies, you may not elect to have an amniocentesis. Although not
compulsory the procedure may ease a parent into their child having lifelong
health problems and may allow them to prepare themselves for the first
encounter with the baby and understand how to take care of he, she or them.
Thank you for reading :)
Written by Anuja Rajeev
·
Links: https://en.wikipedia.org/wiki/Amniocentesis
·
https://www.nhs.uk/conditions/amniocentesis/
·
https://www.nhsinform.scot/tests-and-treatments/biopsies/amniocentesis


Comments
Post a Comment